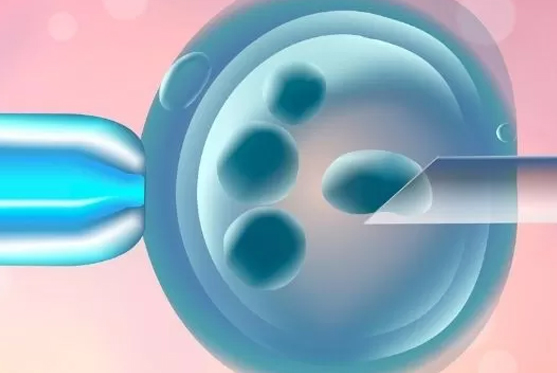
Preimplantation Genetic Testing (PGT) is an advanced IVF procedure used to identify genetic conditions or chromosomal abnormalities in embryos before implantation. By selecting healthy embryos, PGT improves the chances of a successful pregnancy and a healthy baby. It includes two main techniques: PGD (diagnosis) and PGS (screening), with PGT-A being a more refined form of aneuploidy testing.
PGT-A checks for chromosomal abnormalities (aneuploidy), ensuring embryos have the correct number of chromosomes (46). This reduces risks of conditions such as Down Syndrome (extra chromosome 21) or Turner Syndrome (missing an X chromosome).
PGT-M detects single-gene mutations that can lead to inherited disorders, helping prevent transmission of genetic diseases to the child.